Admittedly, the case for re-institutionalization seems grim, if not cruel. The notion of sending a stranger — let alone a family member — to what was once a glorified “human zoo” is enough to strike a visceral chord. But, mental institutions need not be permanently branded with the Mark of Cain. In fact, they need to be reinstated.
The abridged story of institutionalization is as follows: until the late 18th century, mental illness was considered a moral deficiency; a sign that one was intrinsically corrupt. It comes as no surprise, then, that for much of the mentally ill’s harrowing history, they were punished and housed alongside murderers, thieves, and rapists. Indeed, the word “Bedlam” meaning a “state of wild uproar and confusion” has its roots in the Bethlehem Royal Hospital — which mind you, at the time, was considered a progressive institution in 14th century Britain — wherein the mentally ill were bounded in cages and advertised as attractions for bored aristocrats and curious locals.

It would not be until the pioneering work of men like 17th century Paris superintendent Philippe Pinel and his mentor, Jean Baptiste Pussin, that the mentally-ill were reconceived as innocent agents, paralyzed by a mental deficiency — this led to what most historians refer to as the “moral treatment” of the mentally ill. In subsequent decades, chains and cells would be replaced by straitjackets and tight quarters. American physicians like Benjamin Rush — a signatory of the Declaration of Independence — would become diehard proponents of this moral treatment, imploring the public sector to find suitable living conditions for these misfortuned souls. By 1920, there were 20 mental treatment facilities in Massachusetts alone. Such structures were feats of architectural beauty, boasting vast open spaces, well-groomed gardens, and above-average quarters. Still, these facilities could offer little more than custodial care and were mostly staffed by novices largely unaware of standard treatment methods.

The next two decades would witness an abrupt sea-change in public opinion. Professor Emeritus of Psychology at Berkeley, John Kihlstrom, writes that “most public mental hospitals suffered from overcrowding, and budget difficulties which led to a lack of properly trained and supervised staff, and corresponding scandals of the sort exposed by Life magazine in 1946 […] writing that mental asylums were little more than concentration camps.” Yet, there were other factors present — namely the introduction of psychopharmaceuticals that greatly mitigated the symptom profiles of those afflicted with Schizophrenia, Bipolar Disorder, and extreme “Neuroticism.” Also at play was a burgeoning “anti-psychiatry” movement which motivated writers like Thomas Szasz and Professor Theodore Sarbin to declare that mental illness was but a myth — manifestations of “problems in living.”
The combined assault of the above forces propelled mass deinstitutionalization — or an exodus of the mentally ill from their state-sponsored captivity. Dr. Dominic Sisti and Dr. Andrea Segal remarked in a 2015 paper published in the Journal of the American Medical Association (JAMA) that “In 1955, 560,000 patients were cared for in state psychiatric facilities; today there are fewer than one-tenth that number: 45,000.” Given the doubling of the U.S. population, this represents a 95% decline, bringing the per capita psychiatric bed count to about that same as it was in 1850.” But, perhaps, this startling decline is not something at which we should furrow our collective brow. In fact, progressives of the 1960s openly embraced the demise of these “oppressive” institutions. In truth, they believed that the mentally ill would be better of with their family and friends –– flourishing in their newfound autonomy, as Jimmy Carter was fond of arguing.
For many recently freed captives, however, family never came and friends never called. The much ballyhooed abolition almost overnight yielded a new body count of wayward souls forced to take to the streets without care, housing, or even a reliable source of food and water. In an updated-tracker study by the Treatment Advocacy Center, 27-36% of those individuals who were discharged from mental institutions in Ohio and Massachusetts were indicated as homeless or “had no known address” within 6 months of release. Currently, metrics suggest that the percentage of homeless that have received treatment for mental illness is 45% — that number is likely to be higher dependending on the time of testing. More conservative estimates suggest that at least 33% of the nation’s homeless are plagued by “severe mental illness.” (Of course, mental illness is not the sole contributor to transience — other contributors including outstanding drug addiction, cyclical poverty, familial abuse, and human trafficking too take their toll.) Often, these tortured men and women rarely get the help, medication, or housing that they deserve and want — upwards of 97% indicate that they are trying to find housing but struggle because of bureaucratic red-tape. Instead, many end up as downtrodden beneficiaries of poorly staffed and poorly funded non-profit and state-sponsored collectives that offer even less than the mental institutions of yesteryear. As a result, such individuals are put at risk for drug abuse, crime, and a whole-host of unintentional misdemeanors. A 2001 study of 5,000 homeless by the University of Pennsylvania concluded that they cost taxpayers approximately $40,500 per annum “for their use of emergency rooms, psychiatric hospitals, shelters and prisons.”
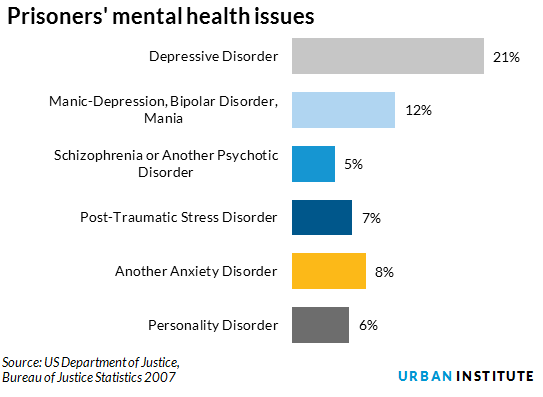
I believe the latter factor is most troubling. The TAC reports that an estimated 15% of those in jails and 20% of those in state-prisons suffer from some form of severe mental illness. Taken prima facie, TAC finds that “this [figure] is 10 times more than the approximately 35,000 individuals with serious mental illness remaining in state hospitals.” Remember, these individuals are not afflicted with run-of-the-mill depression or OCD, at least 10% of those who volunteered in a 2006 Department of Justice jail (not prison) survey displayed symptoms that “met the criteria for psychosis.” The report went on to argue that “this survey was based on 2004 data and the situation has gotten worse since then. Thus, “15 percent would appear a conservative estimate.” In the course of 200 years of mental illness reform, we have cycled back to almost the exact same place — the mentally ill are treated as criminals or forced to live as vagrants.
In the face of such horrifying statistics, it is clear that something has gone awry. While de institutionalization seemed the “ethical choice” almost fifty years prior, its absence has had an indisputably detrimental effect on the lives of the nation’s most burdened citizens. It is time that the government take back the reigns from inept community and impoverished state-run organizations alike and re-institutionalize; this time, setting up a humane system that’s properly funded and staffed by competent caretakers.
Is cost your concern? Then, I would like to point out two salient factors: First, the prison system costs the nation upwards of $39 billion annually; we also know that somewhere between 50-70% of the prison population is afflicted with some form of mental illness. Second, the department of Housing and Urban Development (HUD) estimates that the average homeless person (45% or ~250,000, of which are likely mentally-ill) costs taxpayers almost $40,000 per year. Even if you consider what is “morally just” wholly irrelevant, it seems at least tempting to consider the alternative for purely economic reasons.
But, what about those that will inevitably refuse help, medication, or even housing? The legal standard, as articulated by the Mental Illness Policy Organization (MIPO), remarks that the state will have grounds to commit someone for two reasons: “The first is to protect the citizenry from harm (“police powers”) and the second is to protect the individual from harming himself (“parens patriae”). While the “parens patriae” power has languished in recent years, some legal scholars have suggested that it is time for the law be reinvigorated in order to deal with the burgeoning crisis at hand. The potential for authoritarianism does not escape your author’s purview –– such legislative steps will have to be fleshed-out within a revised legal framework.
Re-institutionalization was once a horror — its future need not be so. If humane and just treatment is what we seek, then the nation must accept that it cannot keep turning a blind eye to the structural injustices that continue to besiege those plagued by mental illness.
Featured Image Source: Open Minds





One Comment